Listen to a podcast on the presentation, etiology, precipitants, management and disposition of Atrial Fibrillation in the Emergency Department from the Emergency Medicine Cases.
Click on the link for the podcast.
And listen to another podcast (click here) on interview with Ian Stiell
Some of my take-home points and additional highlights from the Canadian Cardiovascular Society (CCS) AF Guidelines (2014 focused update and 2010):
Three considerations to take into account when considering whether to rate-control or rhythm-conversion (in stable cases LESS THAN 48 hours unless properly anticoagulated for 3 - 4/52):
1. Age: younger age, more likely for rhythm control, Younger patients tend to be more symptomatic
2. Symptoms: the more symptomatic, the more preferable for cardioversion
3. Recurrence: The higher the likelihood of recurrence, the less preferable for cardioversion. May consider ablation in these cases.
Source: Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: Rate and Rhythm Management. Click here
Download the Canadian Cardiovascular Society (CCS) Atrial Fibrillation Guidelines 2010: Rate and Rhythm Management. Click here
Download the 2014 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Click here.
The AFFIRM trial showed no benefit in rhythm control vs. rate control in terms of morbidity and quality of life. A slightly higher rate of ischemic stroke in the rhythm group compared to rate-control group especially after the rhythm-controlled patients stopped warfarin or had subtherapeutic INRs. This shows the importance of maintaining anti-coagulation in this group of patients with rhythm-control. A word of caution in interpreting the results of the AFFIRM trial: the fairly healthy and young patients were excluded from the study (minimum age in the AFFIRM trial is 65 y/o; mean, 70 y/o). Click here for the AFFIRM trial.
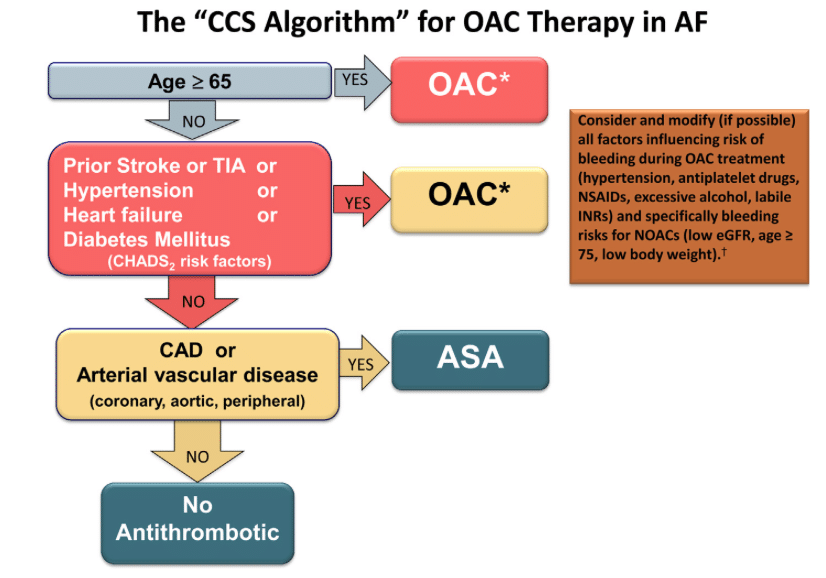
New Algorithm from the Canadian Cardiovascular Society Guideline for AF 2014
Target for rate-control:
In the CCS 2010 guidelines the target is to bring to a resting heart rate of < 100 bpm based on randomized clinical trial data suggesting no difference between strict and lenient rate control targets.
Medications for rate control:
1. Beta-blocker (works in 70% of patients) - metoprolol, e.g.
2. Calcium channel blockers (works in 54% of patients). E.g. Diltiazem
All these drugs act by slowing AV nodal conduction and prolonging AV nodal refractoriness
In the 2010 guidelines, digoxin was downgraded to second-line therapy for rate control of AF, behind calcium channel blockers and β-blockers. Specifically, we suggested that “digoxin not be used as initial therapy for active patients and be reserved for rate control in patients who are sedentary or who have left ventricular dysfunction.
Why Digoxin is less effective compared to beta-blockers and CCB in rate-control? According to CCS AF Guidelines 2010:
Digoxin is poor at controlling rate during exercise or anxiety states because the mechanism of action of digoxin is to increase the AV nodal refractoriness through vagal stimulation.
But during exercise and states of increased sympathetic stimulation, the vagal tone is dampened, thus digoxin is less effective in controlling heart rate than beta-blocker or CCB.
Furthermore, digoxin takes a longer time to act.
Digoxin should not be given as the sole agent in active patients.
Chemical cardioversion
A. Those patients with NO structural heart disease/coronary heart disease:
1. Flecainide (most effective; 80% within 6 hours success rate)
2. Propafenone (can be used as a pill-in-a-pocket approach)
3. Procainamide
Propafenone and flecainide (Class 1 agents) must be combined with an AV nodal blocking agent in order to avoid paradoxically increasing the ventricular rate.
According to the CCS 2010 Guidelines:
B. Those with structural/coronary heart disease:
1. Amiodarone - the only rhythm control drug to be used in ventricular failure/pulmonary oedema
because of its low risk of proarrhythmia in heart failure”Click on the link for the podcast.
And listen to another podcast (click here) on interview with Ian Stiell
Some of my take-home points and additional highlights from the Canadian Cardiovascular Society (CCS) AF Guidelines (2014 focused update and 2010):
Three considerations to take into account when considering whether to rate-control or rhythm-conversion (in stable cases LESS THAN 48 hours unless properly anticoagulated for 3 - 4/52):
1. Age: younger age, more likely for rhythm control, Younger patients tend to be more symptomatic
2. Symptoms: the more symptomatic, the more preferable for cardioversion
3. Recurrence: The higher the likelihood of recurrence, the less preferable for cardioversion. May consider ablation in these cases.
Download the Canadian Cardiovascular Society (CCS) Atrial Fibrillation Guidelines 2010: Rate and Rhythm Management. Click here
Download the 2014 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Click here.
The AFFIRM trial showed no benefit in rhythm control vs. rate control in terms of morbidity and quality of life. A slightly higher rate of ischemic stroke in the rhythm group compared to rate-control group especially after the rhythm-controlled patients stopped warfarin or had subtherapeutic INRs. This shows the importance of maintaining anti-coagulation in this group of patients with rhythm-control. A word of caution in interpreting the results of the AFFIRM trial: the fairly healthy and young patients were excluded from the study (minimum age in the AFFIRM trial is 65 y/o; mean, 70 y/o). Click here for the AFFIRM trial.
New Algorithm from the Canadian Cardiovascular Society Guideline for AF 2014
Target for rate-control:
In the CCS 2010 guidelines the target is to bring to a resting heart rate of < 100 bpm based on randomized clinical trial data suggesting no difference between strict and lenient rate control targets.
Medications for rate control:
1. Beta-blocker (works in 70% of patients) - metoprolol, e.g.
2. Calcium channel blockers (works in 54% of patients). E.g. Diltiazem
All these drugs act by slowing AV nodal conduction and prolonging AV nodal refractoriness
In the 2010 guidelines, digoxin was downgraded to second-line therapy for rate control of AF, behind calcium channel blockers and β-blockers. Specifically, we suggested that “digoxin not be used as initial therapy for active patients and be reserved for rate control in patients who are sedentary or who have left ventricular dysfunction.
Why Digoxin is less effective compared to beta-blockers and CCB in rate-control? According to CCS AF Guidelines 2010:
Digoxin is poor at controlling rate during exercise or anxiety states because the mechanism of action of digoxin is to increase the AV nodal refractoriness through vagal stimulation.
But during exercise and states of increased sympathetic stimulation, the vagal tone is dampened, thus digoxin is less effective in controlling heart rate than beta-blocker or CCB.
Furthermore, digoxin takes a longer time to act.
Digoxin should not be given as the sole agent in active patients.
Chemical cardioversion
A. Those patients with NO structural heart disease/coronary heart disease:
1. Flecainide (most effective; 80% within 6 hours success rate)
2. Propafenone (can be used as a pill-in-a-pocket approach)
3. Procainamide
Propafenone and flecainide (Class 1 agents) must be combined with an AV nodal blocking agent in order to avoid paradoxically increasing the ventricular rate.
According to the CCS 2010 Guidelines:
“Class I drugs, such as flecainide and propafenone, block sodium channels. This slows atrial conduction, lengthens atrial refractoriness, and suppresses automaticity. By destabilizing AF-maintaining rotors, this class of drugs can prevent the persistence of AF. Class I agents slow the atrial rate in AF by slowing conduction in reentrant rotors or wavelets. The ventricular response to AF is determined by complex interactions between the rate and pattern of activation of the proximal AV node from the atrium on one hand and the refractory properties of the AV node on the other. Because of the decremental conduction properties of AV nodal tissue (involving Ca2+-current–dependent action potentials and zones of poor cell-to-cell coupling), atrial impulses that fail to conduct through the AV node leave the node partially refractory to the next impulse, a phenomenon called concealed conduction. Paradoxically, a slowing in atrial rate can therefore cause an increased ventricular response due to a reduction in the number of concealed activations in the AV node. In the most extreme cases with very slow organized atrial activation, conversion of AF to AFL and subsequent 1:1 conduction of AFL can ensue, causing a very high ventricular rate and risk of ventricular tachyarrhythmia. Class I agents (flecainide and propafenone) can increase the risk of ventricular arrhythmias especially in patients with coronary artery disease or left ventricular dysfunction, so these agents should be avoided in these populations.”
B. Those with structural/coronary heart disease:
1. Amiodarone - the only rhythm control drug to be used in ventricular failure/pulmonary oedema
- Takes longer time
- Safe, good at controlling ventricular rate
- CCS 2010 Guidelines: “in patients with left ventricular ejection fraction <35 b="">amiodarone, is the only drug usually recommended
2. Ibutilide
Can be used in structural heart disease but not in ventricular failure
Beware: causes prolonged QT interval
“Pill in the Pocket” Approach for Atrial Fibrillation
Excerpts from the 2010 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation:
"Some patients with symptomatic AF have relatively long-lasting episodes (eg, more than 4 hours) but with long intercurrent periods of sinus rhythm between episodes (eg, less than 2-6 year). In these patients, a strategy of daily therapy may be unnecessary. An alternative possibility is to prescribe oral antiarrhythmic drugs that can be taken at the time of an episode for acute termination of AF. Clinical trial data have shown this “pill in the pocket” strategy to be both safe and effective. The drugs most commonly used for this purpose are class I agents given as a single dose at the onset of AF. Flecainide is given as a single or cumulative 200 to 300-mg dose, and propafenone is given as a single 450 to 600-mg dose. Both these agents have a 50% to 80% efficacy in acutely terminating AF. Some physicians also prescribe a rapidly acting beta-blocker (eg, metoprolol 50 to 100 mg), to be taken at the same time as the class I antiarrhythmic agent in order to minimize the risk of accelerating the ventricular response."
Commonly used criteria: CHADS2 score
IF CHADS2 score is 0, proceed to use CHA2DS2VACs for a more refined decision on stroke risk stratification.
Image source: http://www.afnewjersey.com/images/anticoagulation.png
Excerpts from the 2014 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation:
"In the 2010 and 2012 CCS guidelines, it was recommended that the Congestive Heart Failure, Hypertension, Age, Diabetes, Stroke/Transient Ischemic Attack (CHADS2) schema be used to estimate stroke risk, because of its simplicity, familiarity, and extensive validation.
However, in the 2012 guidelines, elements of the Congestive Heart Failure, Hypertension, Age (≥ 75 years), Diabetes, Stroke/Transient Ischemic Attack, Vascular Disease, Age (65-74 years), Sex (Female) (CHA2DS2-VASc) schema were incorporated in an algorithm for the selection of antithrombotic therapy, particularly for patients with a CHADS2 score of 0.
For 2014, the CCS continues to recommend that the CHADS2 schema be used to estimate stroke risk, complemented by the inclusion of some, but not all, of the CHA2DS2-VASc criteria. [CCS] are recommending an updated simple “CCS algorithm” to select appropriate antithrombotic therapy as below:
Bleeding risk of patients considered anticoagulation
HAS-BLED score
Finally, remember to treat the underlying causes of the AF (if the AF is secondary or a manifestation of an underlying pathology).
In a recent retrospective 1-year study involving 416 patients at two Canadian emergency departments on patients with A-fib/flutter secondary to complex acute medical issues such as thyrotoxicosis, COPD, etc), it is found that among the 135 patients with attempted rate or rhythm control, 41% had adverse events such as hypotension or required intubation whereas among the 281 patients with no attempted rate or rhythm control, 7% had adverse events which suggests that in the presence of an underlying medical condition and when the tachyarrhythmia is an appropriate physiological response of the heart to a medical problem, treating the underlying cause is more important and suppressing the AF may in fact be detrimental.
Additional contents:
A short lecture about WPW and AF:
And a quick revision on antiarrhythmics:





No comments:
Post a Comment